I’m Will Erickson, I work as an organizer and continuous improvement coach with the Labor Management Partnership Office at UMass Memorial Health in Worcester, MA. I’ve attended the Forum several times over the years but this is my first time presenting, and I’m so grateful that my friends Amar and Becka invited me to join them.
Ok, so now I’m going to tell you about how we’re improving how people feel about coming to work every day through our Unit Based Team program at UMass Memorial, in partnership with our largest union.
First, a little bit about our system: we’re a mid-size academic medical center and safety net with a bunch of community hospitals and practices in Central Mass. We’re the largest provider and largest employer in our region, so the quality of our jobs, and our care, really matters to our community. Unless I’m misjudging this audience, I’ll bet a lot of you work in places like this one.
To understand this story you also need to know about the SHARE union, which makes up the other half of our labor management partnership. It’s the largest union because it represents a lot of different job titles, like nursing assistants, medical assistants, rad techs, respiratory therapists and billers. We organized our union around the values of solidarity and voice: taking good care of each other and being able to participate in decisions about what happened to us. I say us because I come out of this union as an organizer. The lead organizer of that union, Janet Wilder, is in the audience this morning.
Coming into 2016, SHARE leaders had achieved a lot in terms of making their jobs better, but they felt that they hadn’t made a lot of progress making these jobs feel better – in a lot of ways, the work felt harder and more draining than it had. Together with UMass Memorial, we found ourselves facing a shared set of problems; a disengaged workforce that resisted changes they perceived as being done to them – no one wants to feel process improved. We suffered from unreliable processes and variable outcomes, pretty bad patient experience scores, and strained labor relations. And that’s a picture of a much younger me manning an informational picket line in front of one of our hospitals, just to prove my labor bonafides.
We looked around for alternatives, and found the Kaiser Permanente Labor Management Partnership, which is still in place today and the most important labor management partnership in place in US healthcare right now, maybe in any industry in the US. With support from Kaiser and its unions, from our own hospital’s leadership which was a couple years into a Lean journey, and drawing inspiration from a couple trips to the IHI Forum, we did something brave and formed our own labor management partnership, one that was built on those central pillars of voice and solidarity, participation and mutual respect and support.
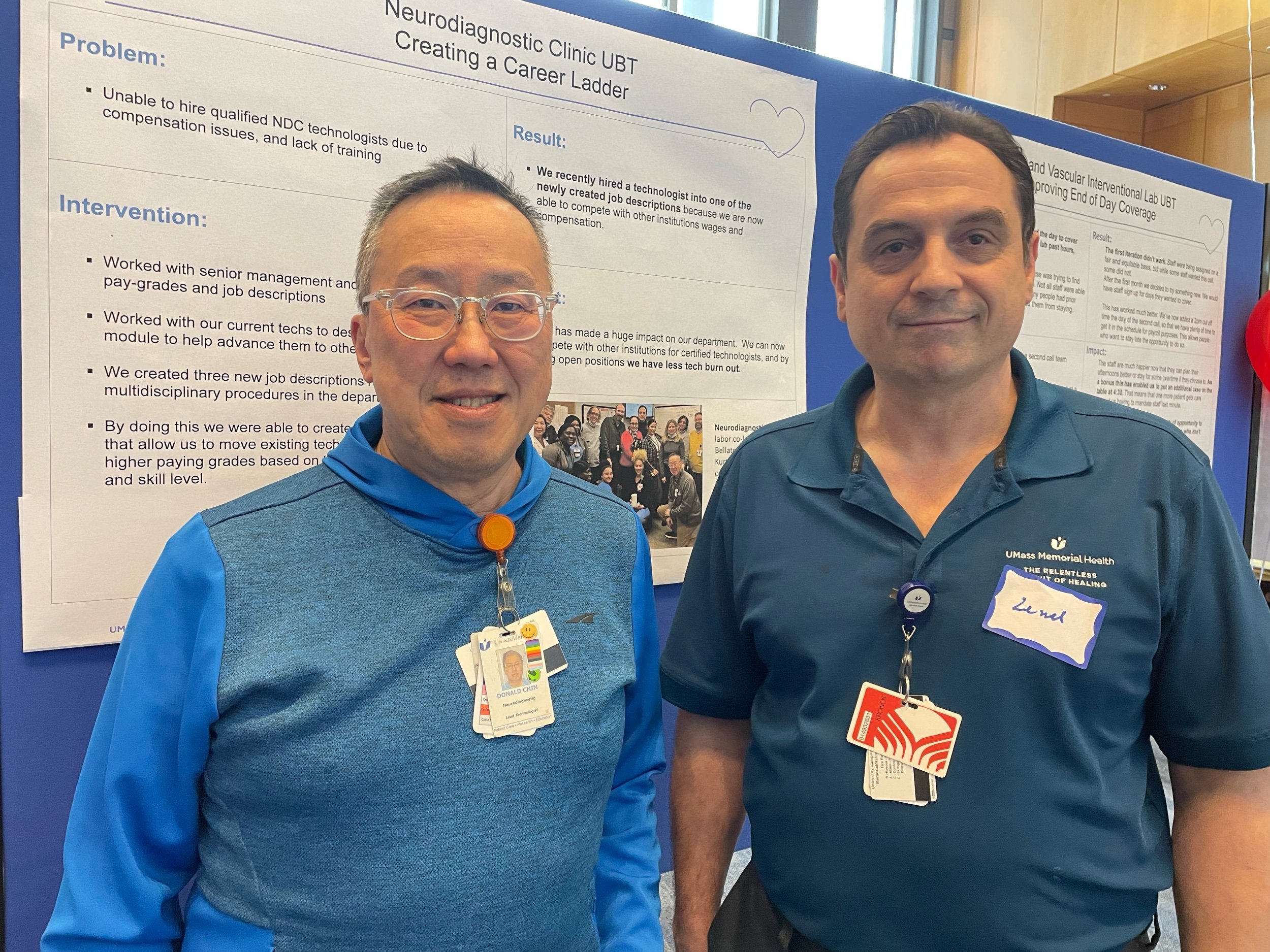
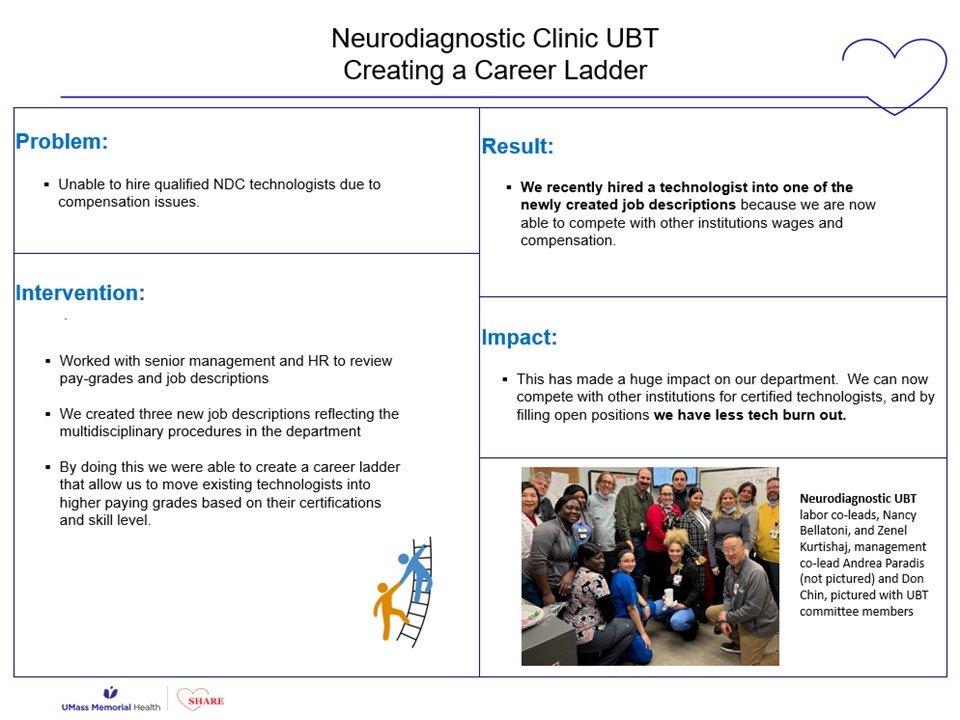
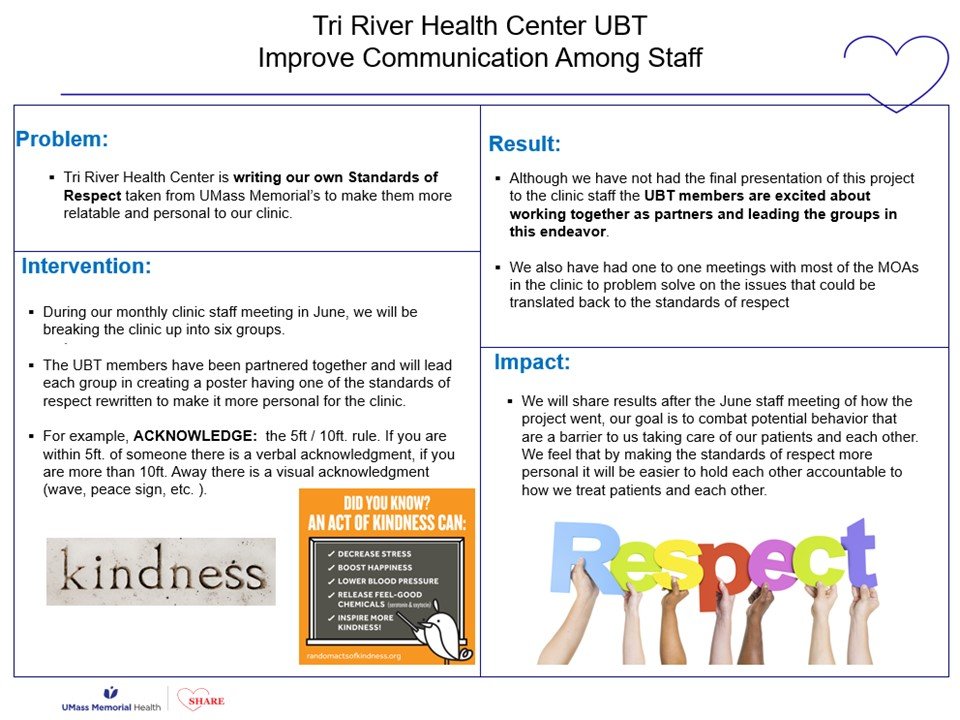
Following the lead of our friends at Kaiser, our Unit Based Teams are built on the foundation of this labor management partnership. These are department-level process improvement teams create to help us establish a more invigorating work culture, to make labor management partnership an actual, real thing at the frontline between staff and their managers and not just for the leaders at the top. This is our effort to organize a bottom up social movement for safer, smoother, better processes.
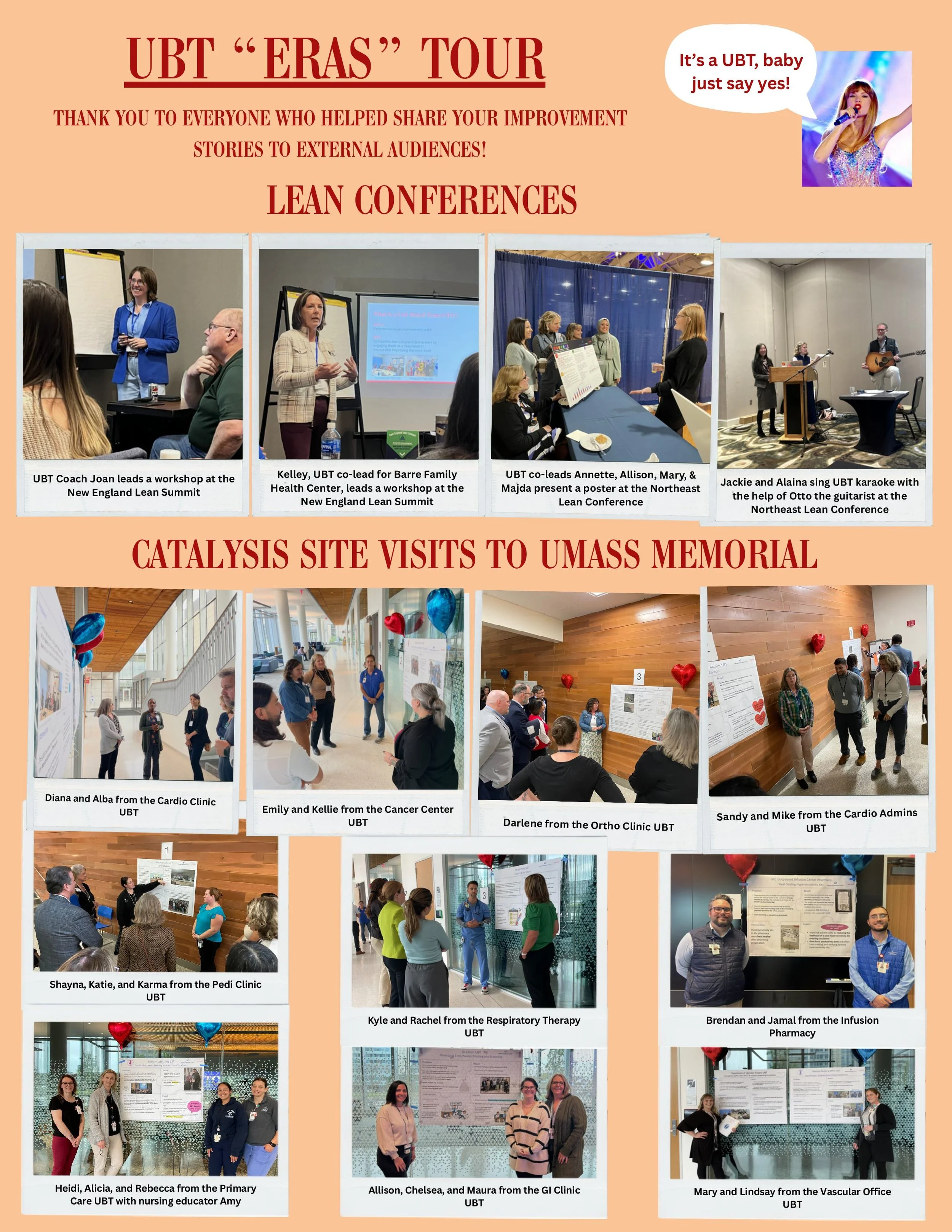
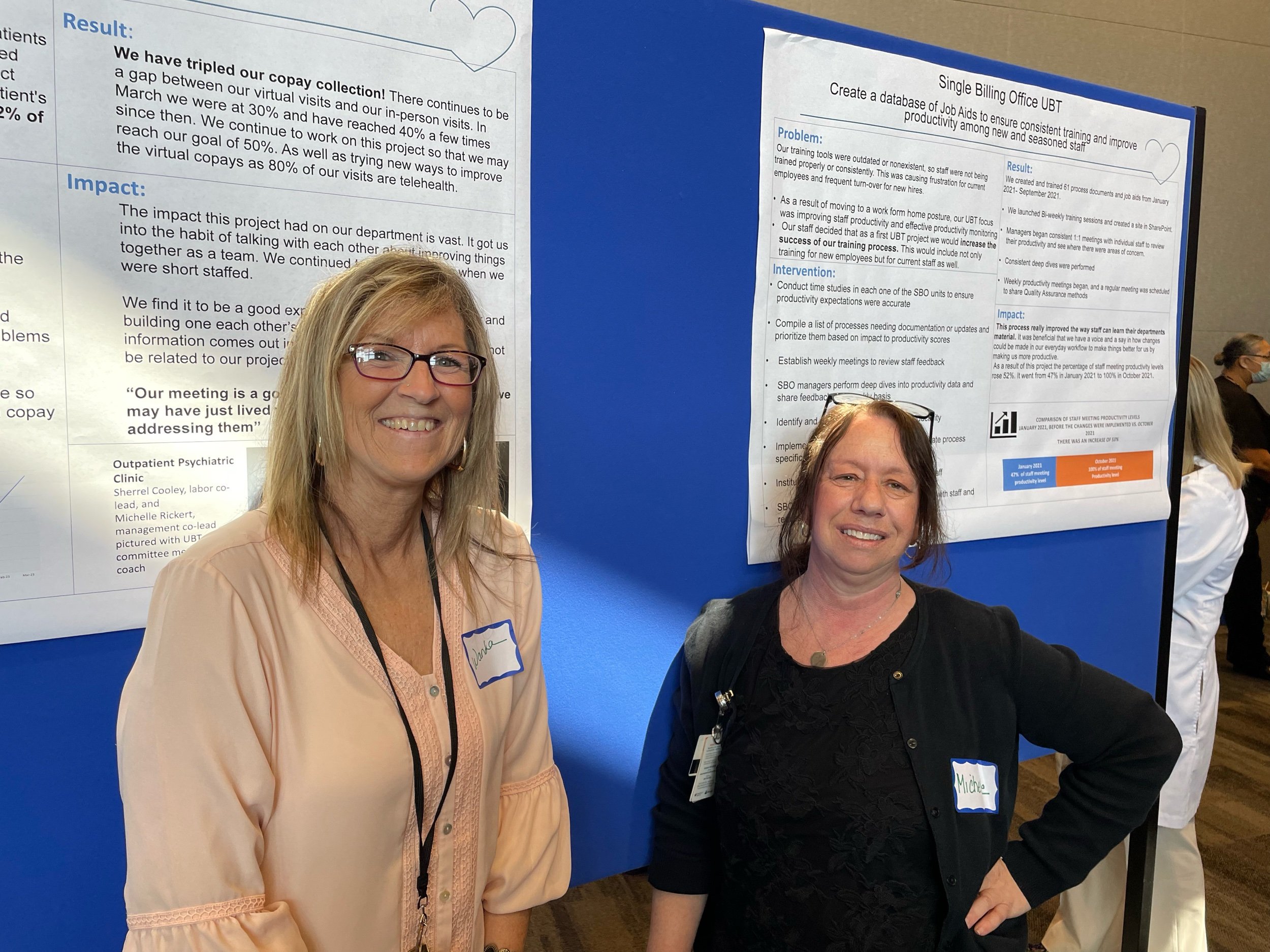
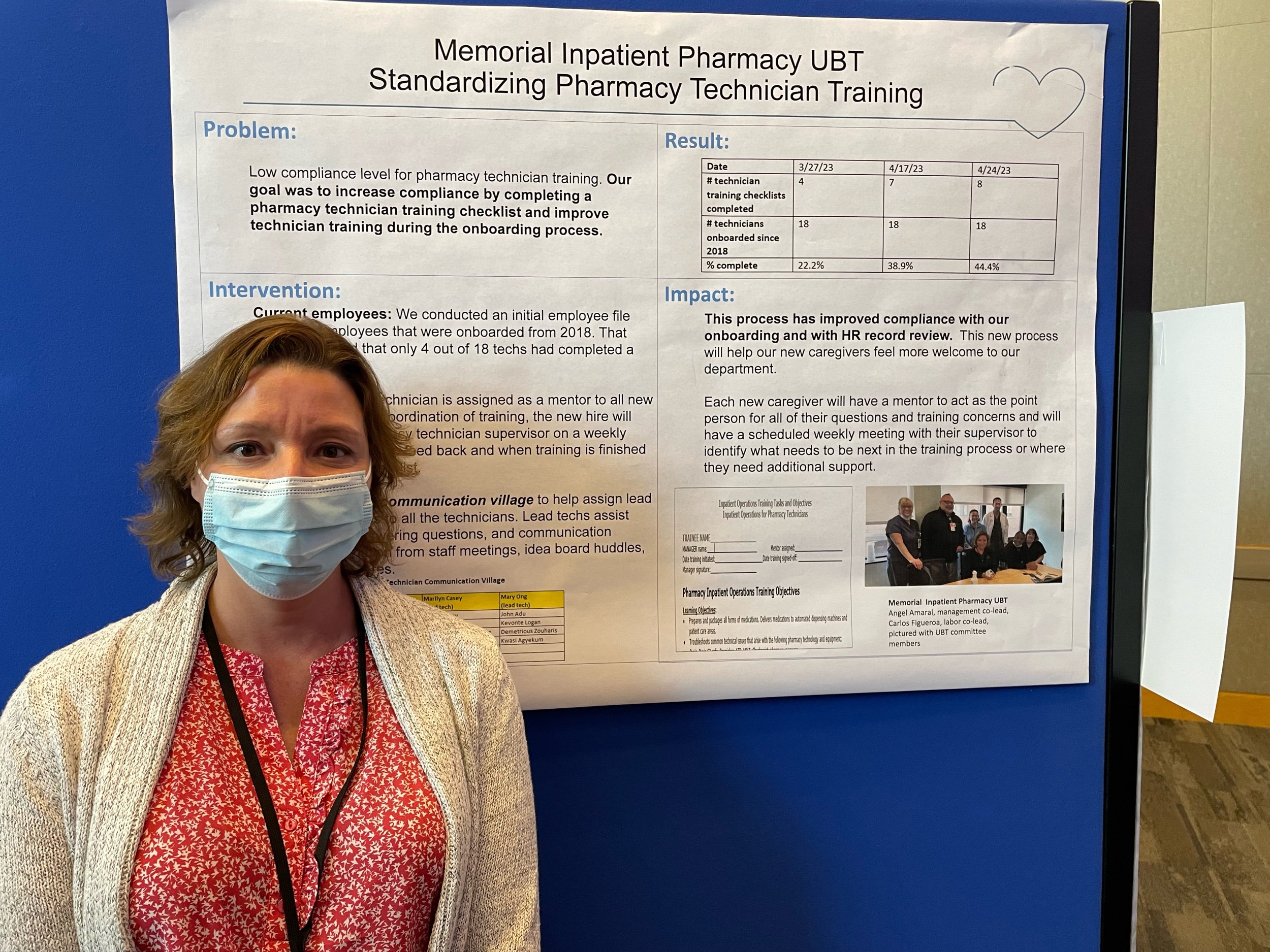
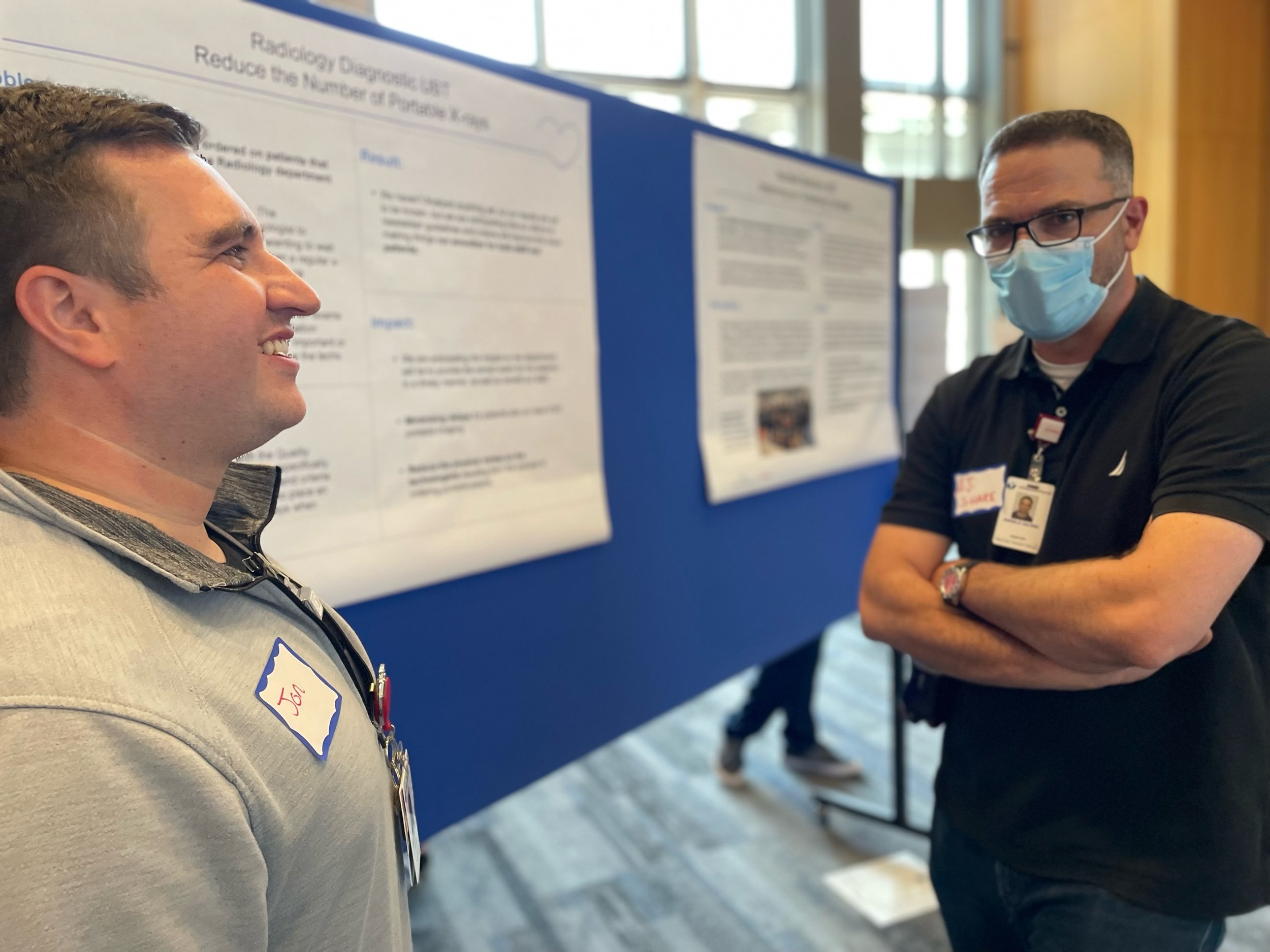
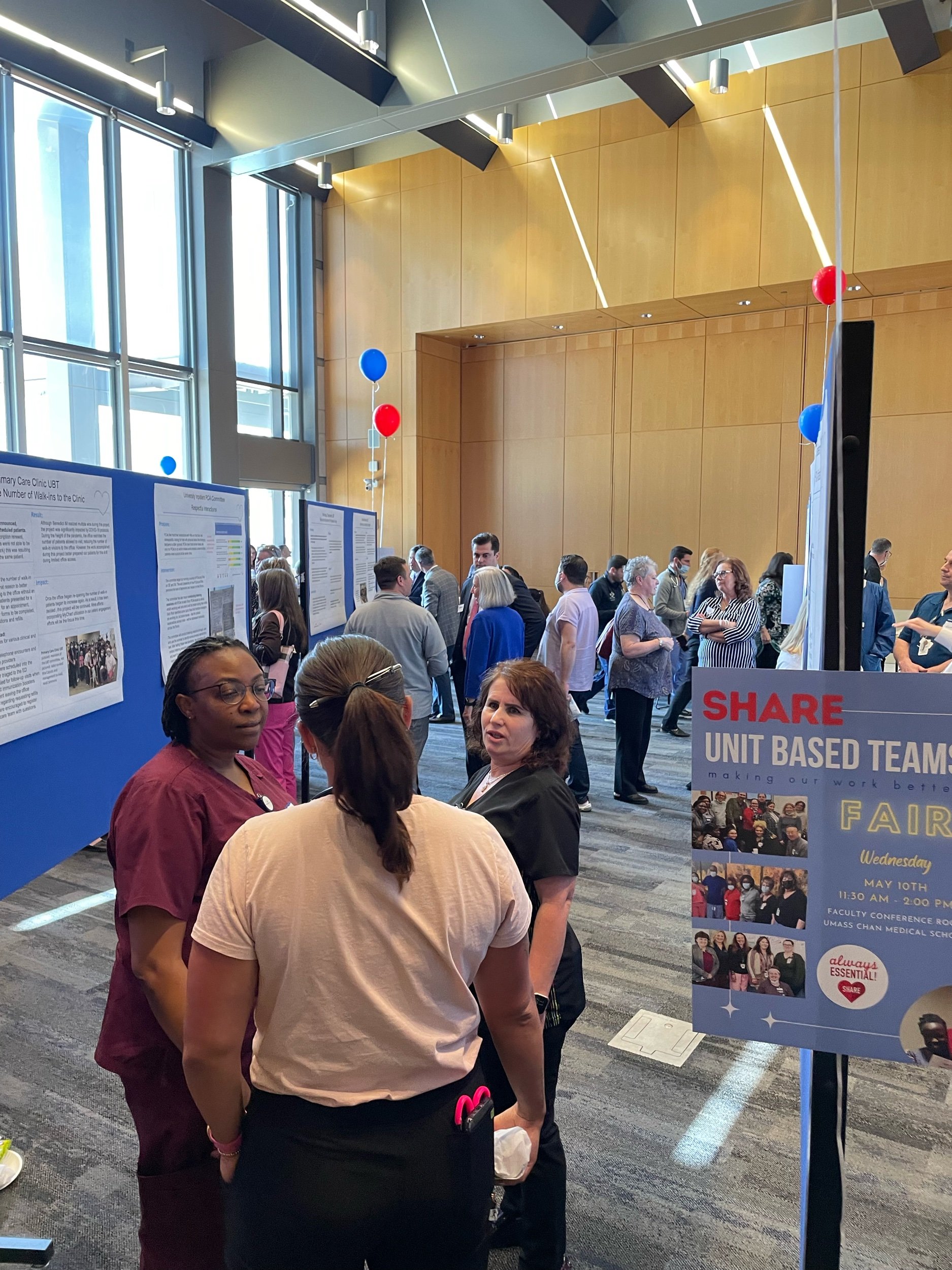
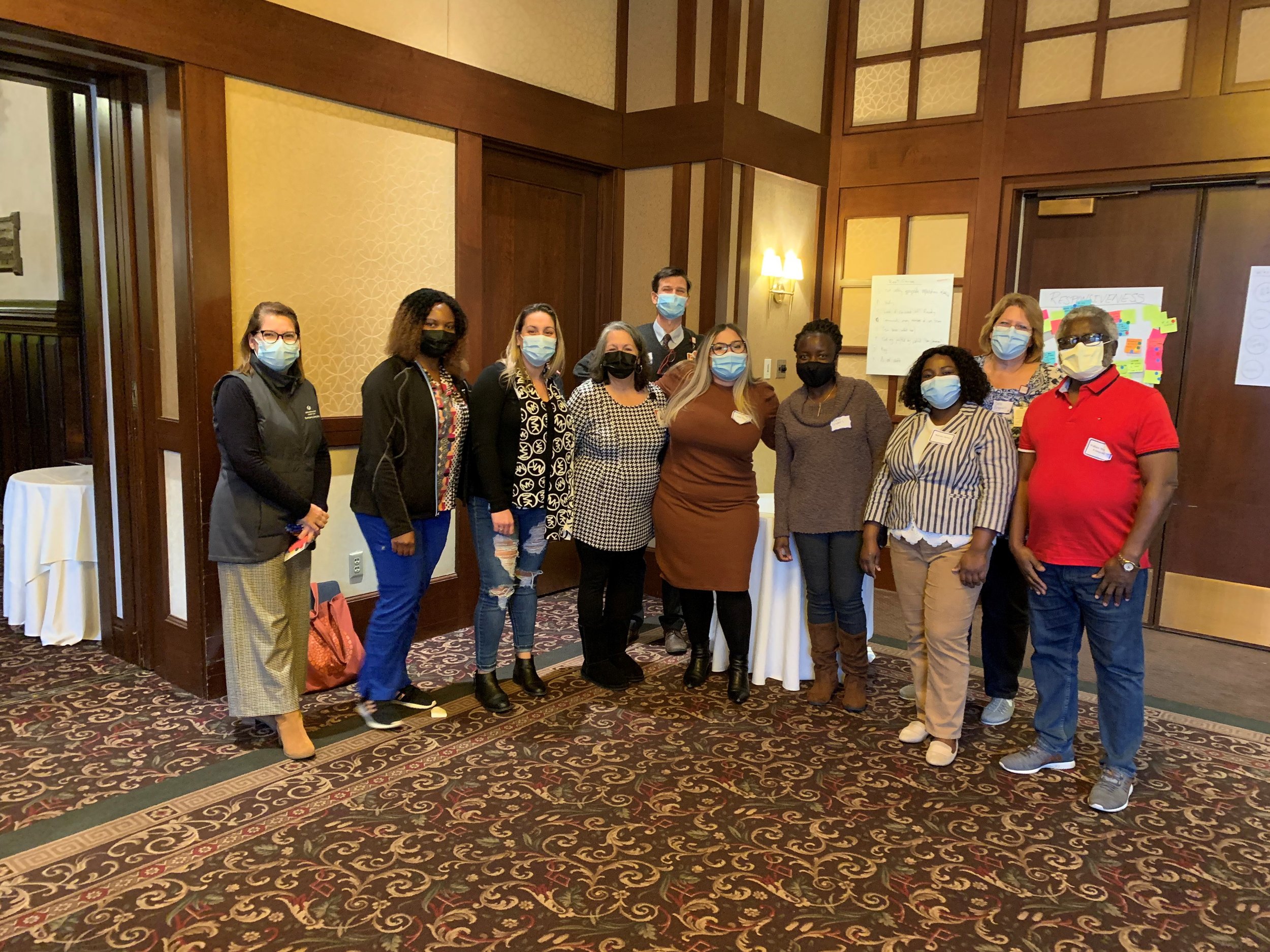
This is a picture of one of our UBT Fairs from last Spring, when we got several hundred of people together to share out posters of their favorite improvement project from the last year. One of the great things about rooting our movement for process improvement in the labor movement is that in the labor movement its still cool to belt out songs together, its one of our proudest traditions. So at these UBT Fairs we actually pass out adapted lyrics to pop songs and get several hundred people to sing together about their love for process improvement.
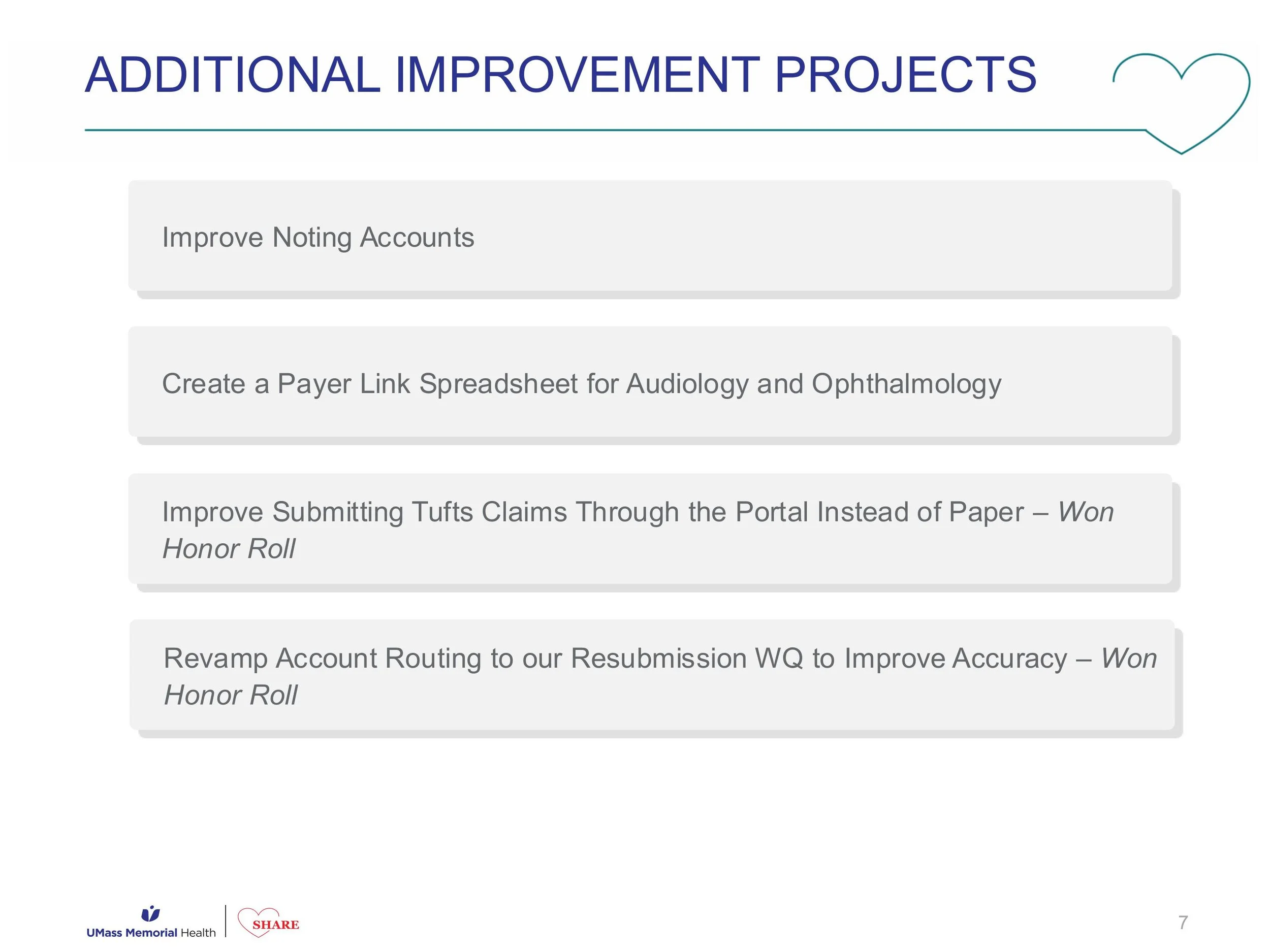
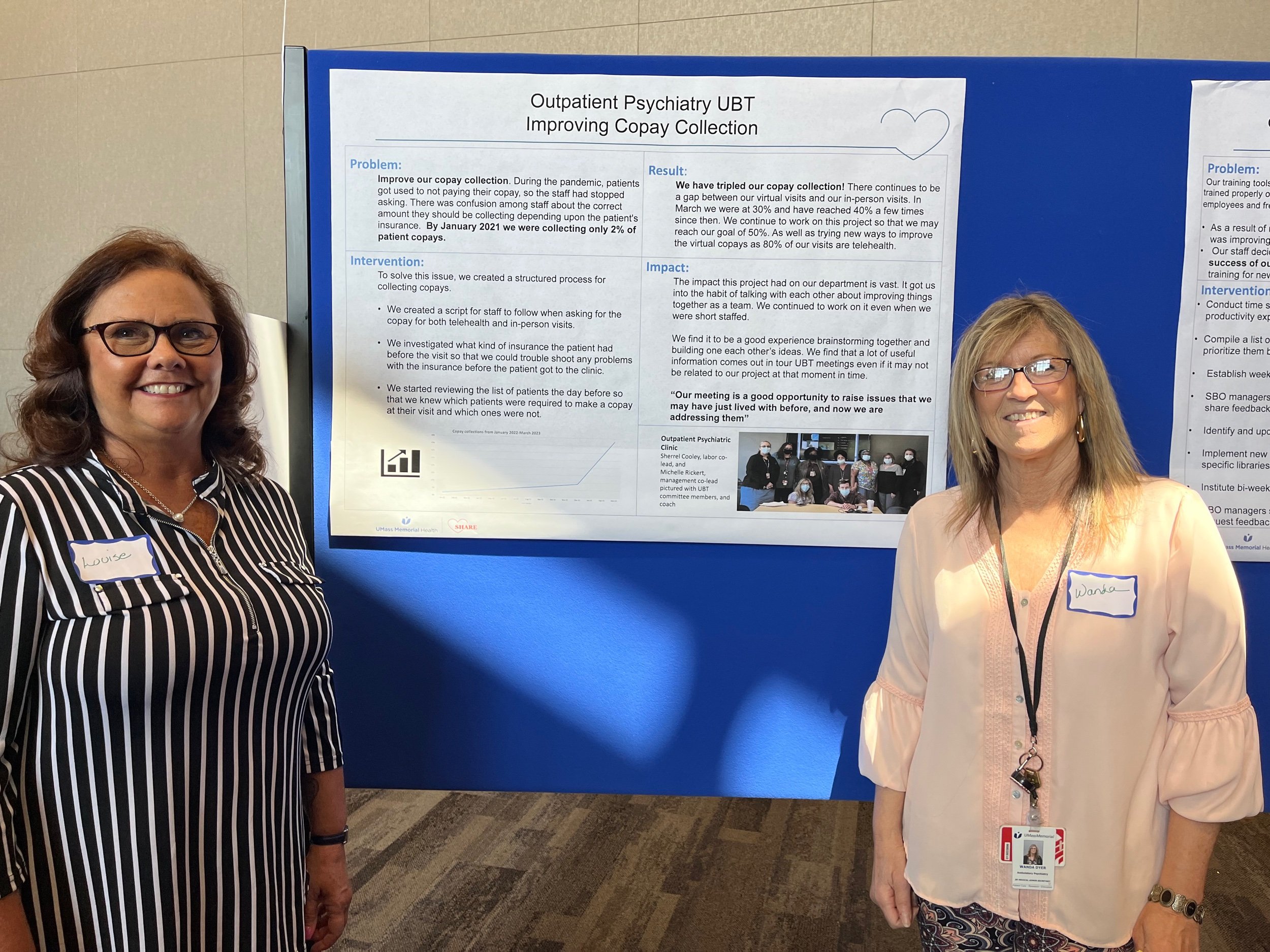
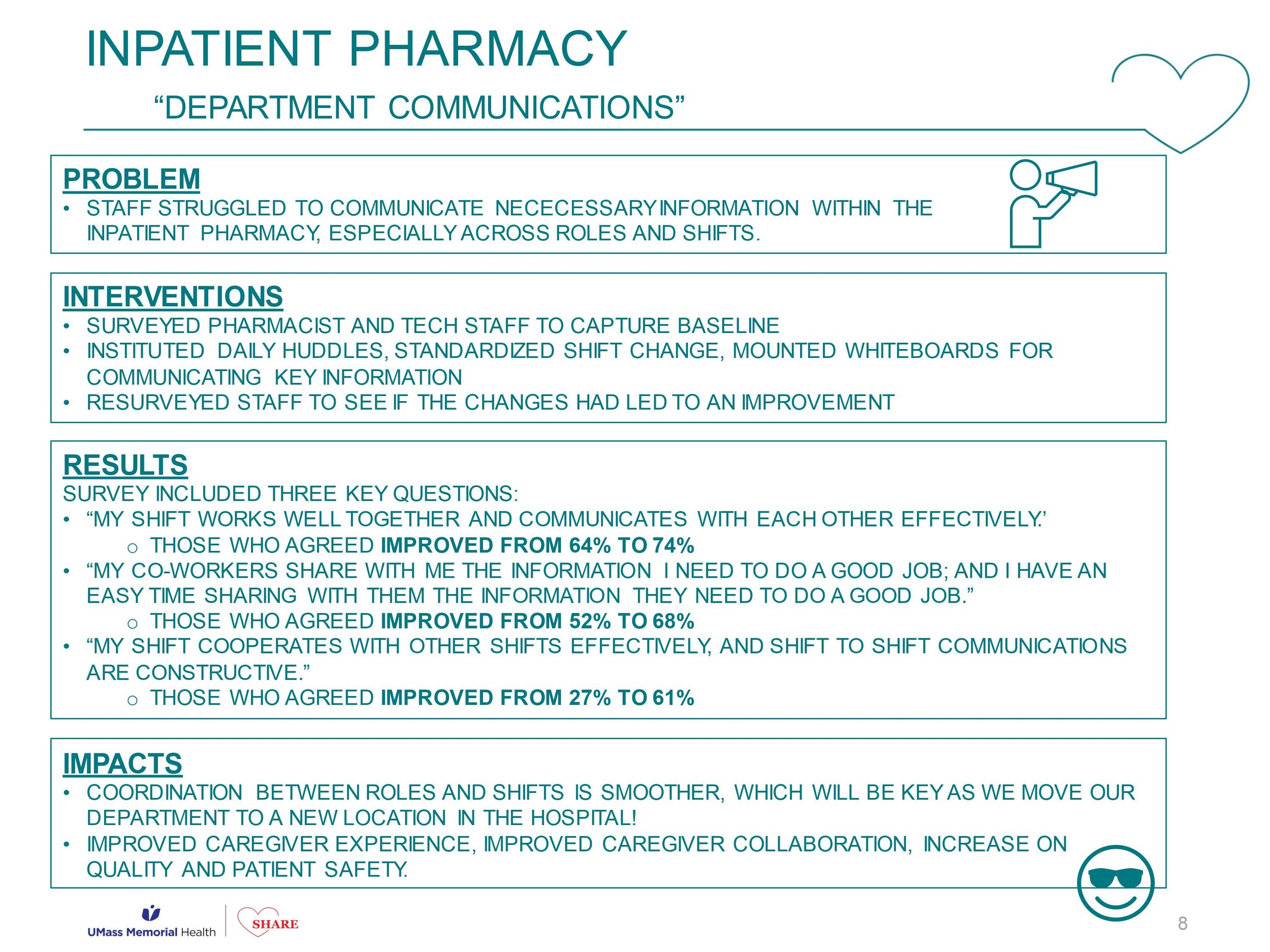
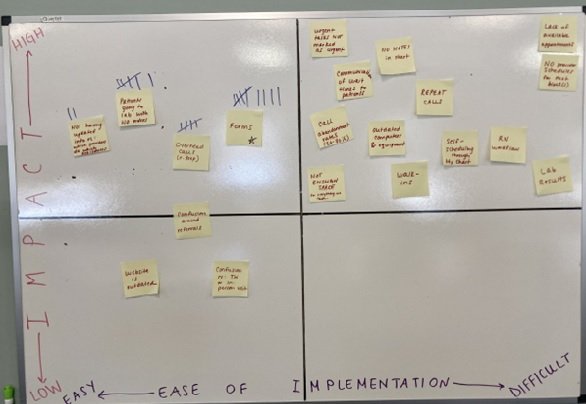
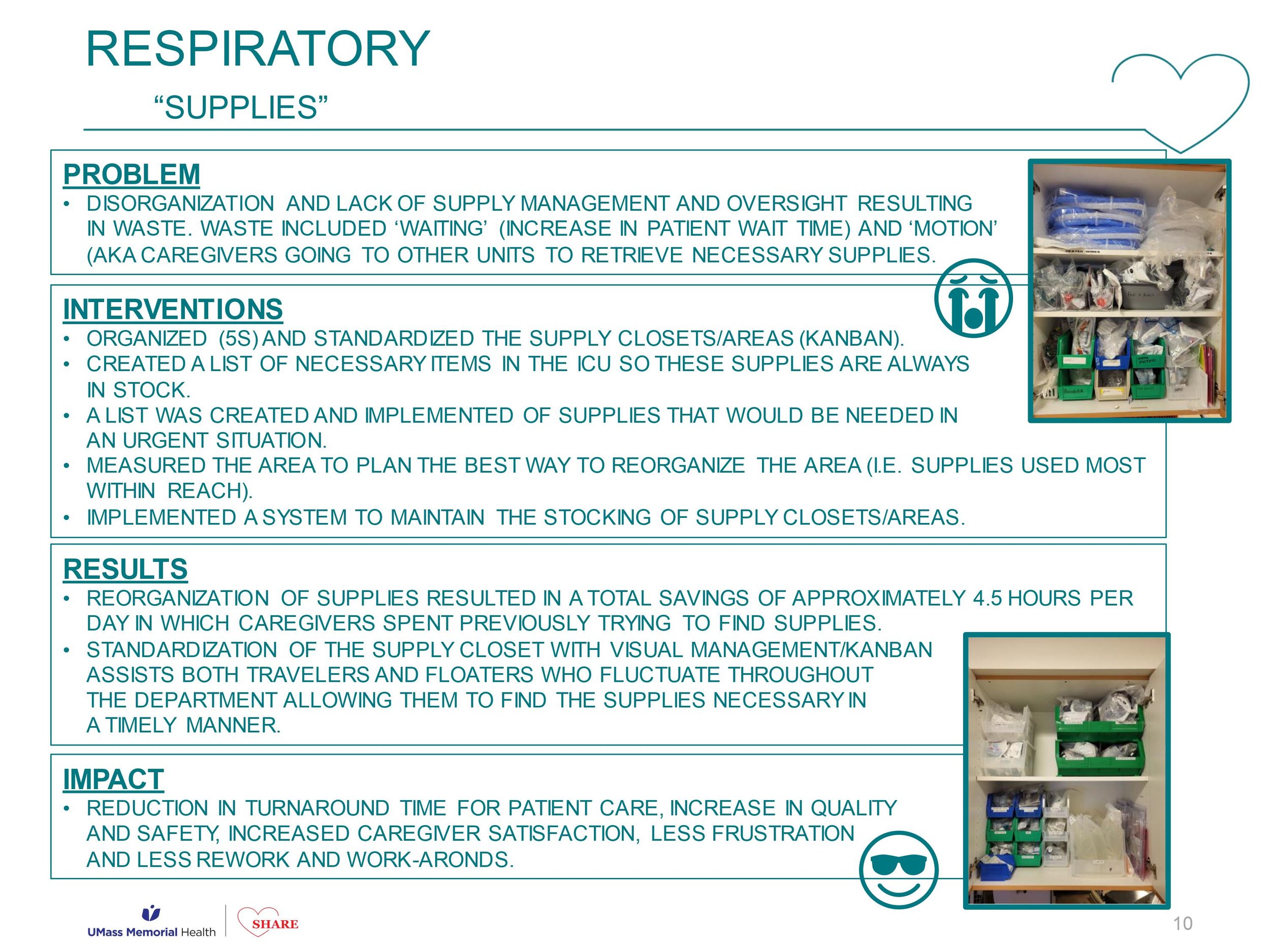
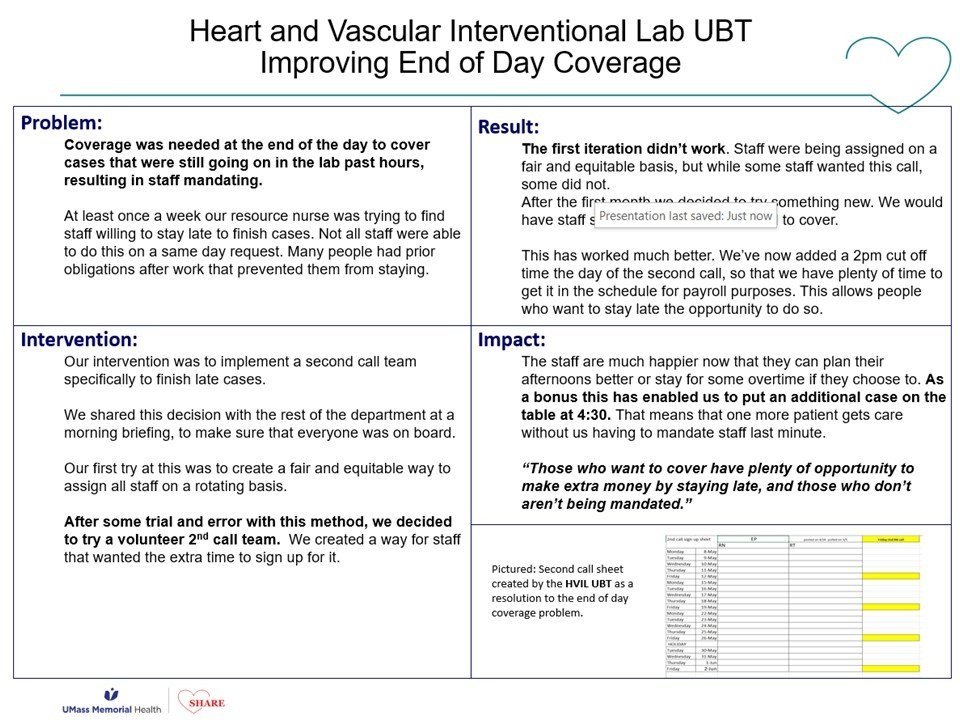
We now have 70 or so UBTs working on projects to reduce falls, to improve patient experience, to reduce no shows, to improve copay collection, to improve throughput. But the UBTs don’t exist for the purpose of solving those problems. The primary purpose of a UBT is to change how our caregivers feel about coming to work everyday. But the big theory of change that animates this whole program for us is that the best way to change how our people feel about their work isn’t pizza parties, or ropes courses, or trust falls, or meditation apps (we’re not against those things) but to involve our frontline people in identifying and then working to solve the process issues that are driving them the most bananas.
Each UBT has a committee of staff, providers and managers. Each is co-led by a labor co-lead and a management co-lead, and each team, in addition to having an improvement coach like me, is co-sponsored by a union leader and a management leader, usually the manager’s boss.
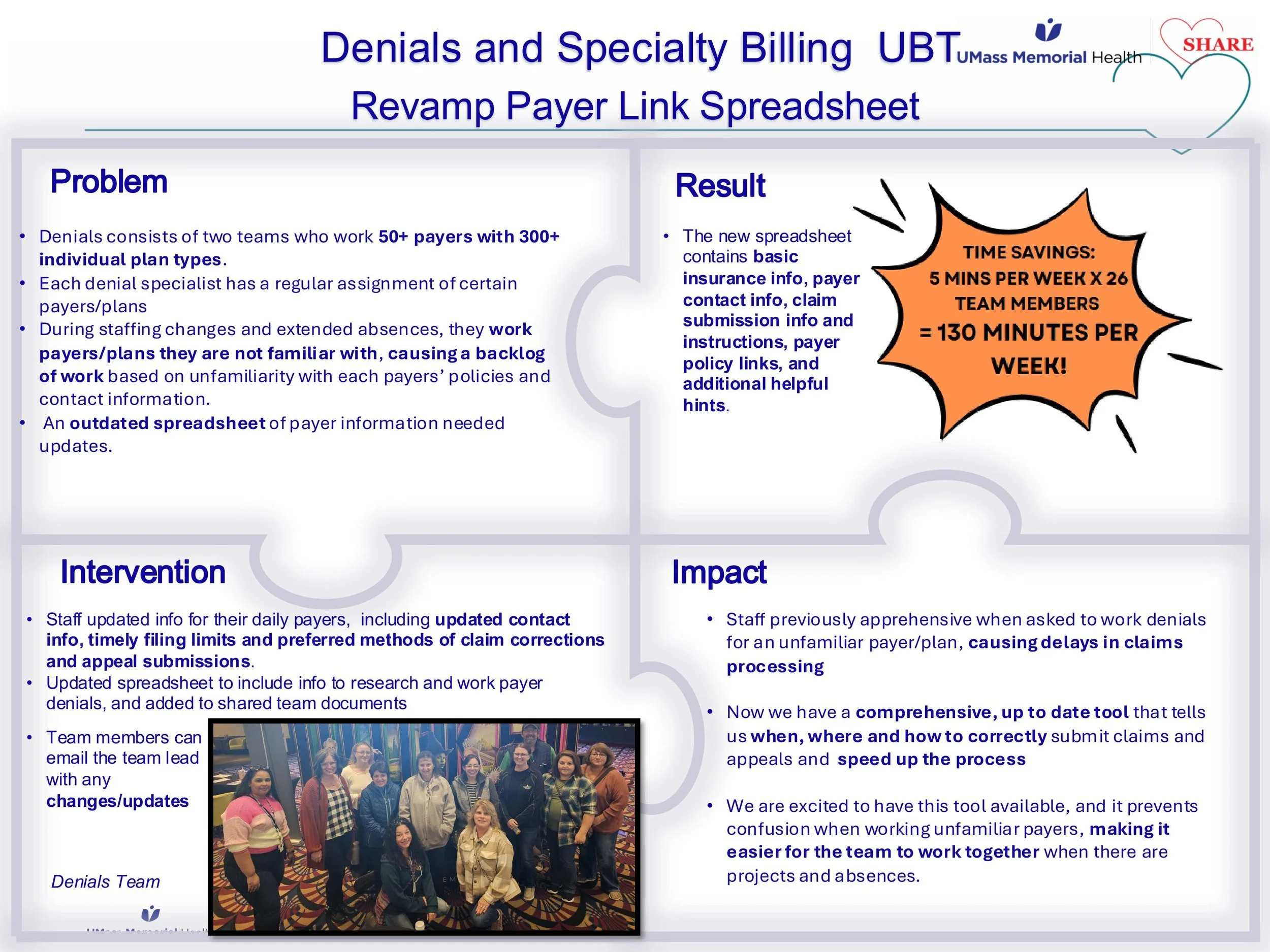
Most of our UBTs meet for 30 minutes every other week, and each works on 2-3 projects at a time. We encourage them to work on big issues, but to scope their project such that it can be completed in less than 100 days – I think that 100 day rule is one we brought back from one of these forums. The co-leads facilitate the meetings and prep for those meetings together beforehand. Our co-leads are really the axle around which the UBT turns, so we give them lots of training and support – we view UBTs as a vehicle for developing frontline leaders and upskilling our managers, not just for process improvement. Projects are chosen by the committee, and decisions are made by consensus. We test for consensus by asking three specific questions: has everyone been heard? Can everyone live with this decision, even if it wasn’t your first or second or third choice – will you try it? And finally, will everyone here support this decision outside this room – are we together in this? We want our improvements to stick.
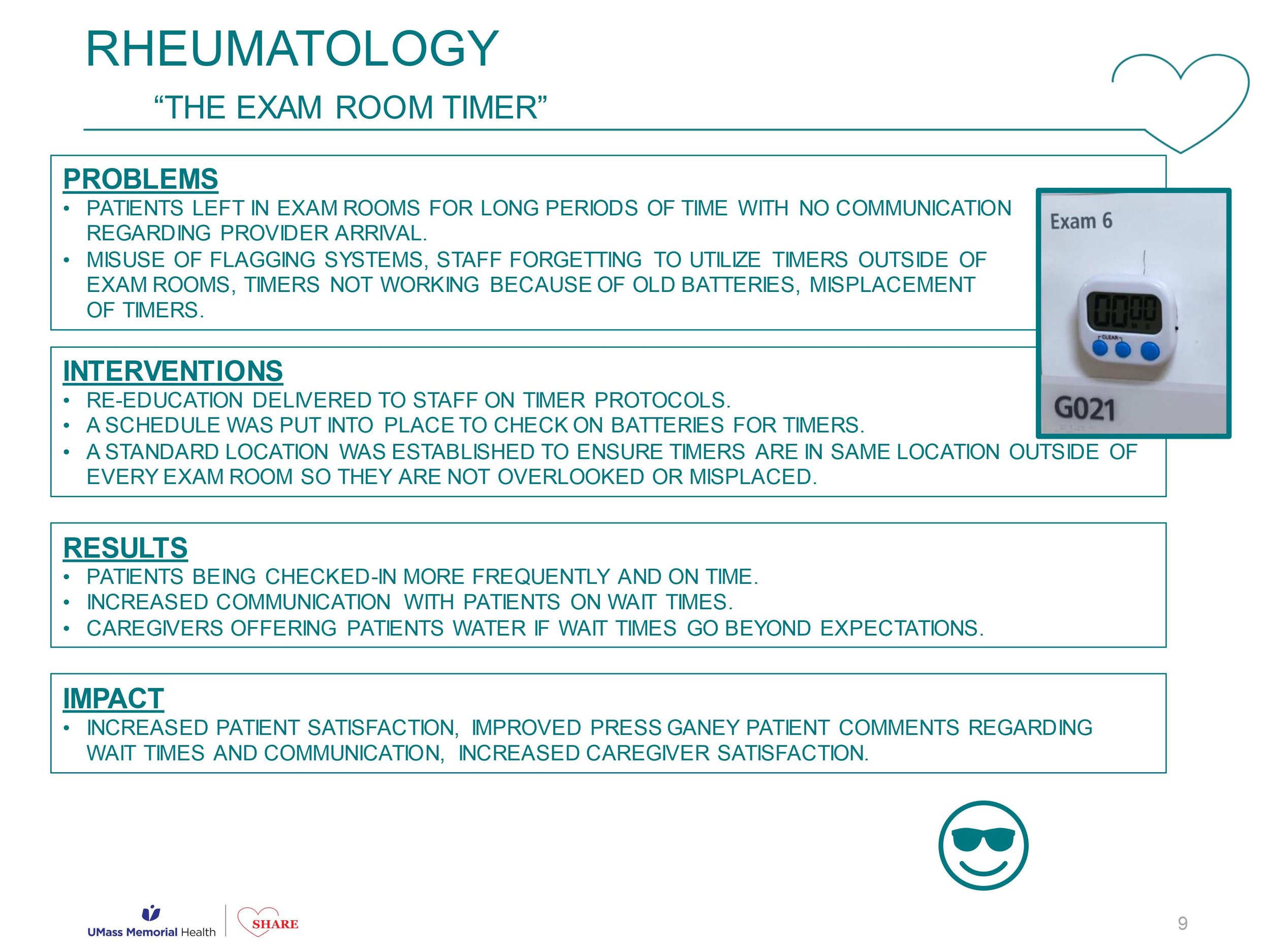
So that’s the concept, but are they actually making a difference? There are several different ways to answer that question. First, our UBTs are making big, substantive impacts with their projects. One of our CT departments, for example, created a patient staging area and reduced wait times by 20% despite an increase in volume. If the management team had gone to the staff and demanded an increase in volume, the techs would have spit the bit – what stressed the techs out more than anything else was how late they were running pulling in outpatients in the afternoons – the techs wanted to see a decrease in outpatient slots. After setting up the staging area, our techs’ reported stress levels were 40% lower. Happier patients and smoother process made happy techs.
Our managers are also reporting general improvements in productivity and good feeling as a result of their UBT work – a kind of generalized halo effect. I love this quote from one of the NPs in Vascular Surgery – this department started out meeting every other week for 30 minutes, then increased that to every week for 30 minutes, and then they extended the time to a full hour because they felt like they were getting so much out of the time together.
And we’re seeing an effect in our caregiver experience survey results as well. In a recent survey departments with a UBT showed twice the improvement in engagement as our entire system, and four times the improvement in the bundle of questions that basically get at what people think of their boss. And the questions with the biggest gap between departments with UBTs and those without one were “I am involved in decisions that affect my work” and “this organization treats employees with respect”. Remember that we built our partnership on the pillars of increasing participation and improving the culture – I just love that.
Our joint improvement work is also gaining notice in the labor relations universe. Here we are with US Secretary of Labor Julie Su. She’s unfortunately only got a few more weeks in the job.
And of course the best evidence that we’re making an impact is what our caregivers are saying about how UBTs have changed them, and how they feel about coming to work. We’re not going to have time to show you this compilation, but we’ll give you the QR code at the end so that you can watch on your phone – I really hope you will.
So to wrap up, what’s different about these UBTs? First, ownership is truly shared. This is not a top down management thing, but its not just a union initiative either. That’s made it easier to leverage multiple leadership networks, especially our often unsung, informal frontline leaders, and sometimes even those grouches in the department who’ve historically been skeptical of any change. We also think we’ve created a structure that makes it easier to talk about hard things – partnership doesn’t mean that we just act nicey-nice to each other. We don’t tiptoe around the hard stuff. We lean into the process issues that are causing conflict, because we want to solve those things. And finally, with every project, every meeting, we’re teaching our people how to work together better and to solve bigger challenges. We’re doing it in a way that refreshes the manager role, positioning them as mentors and leaders, not just command and control authoritarians. And we’re challenging union reps to not just complain that management hasn’t fixed something yet, but to jump in and organize their coworkers to come up with a better way. And we’re doing it in a way that strengthens psychological safety and combats against of the real power imbalances that can make working in a team so hard.