Creating Unity through the Union
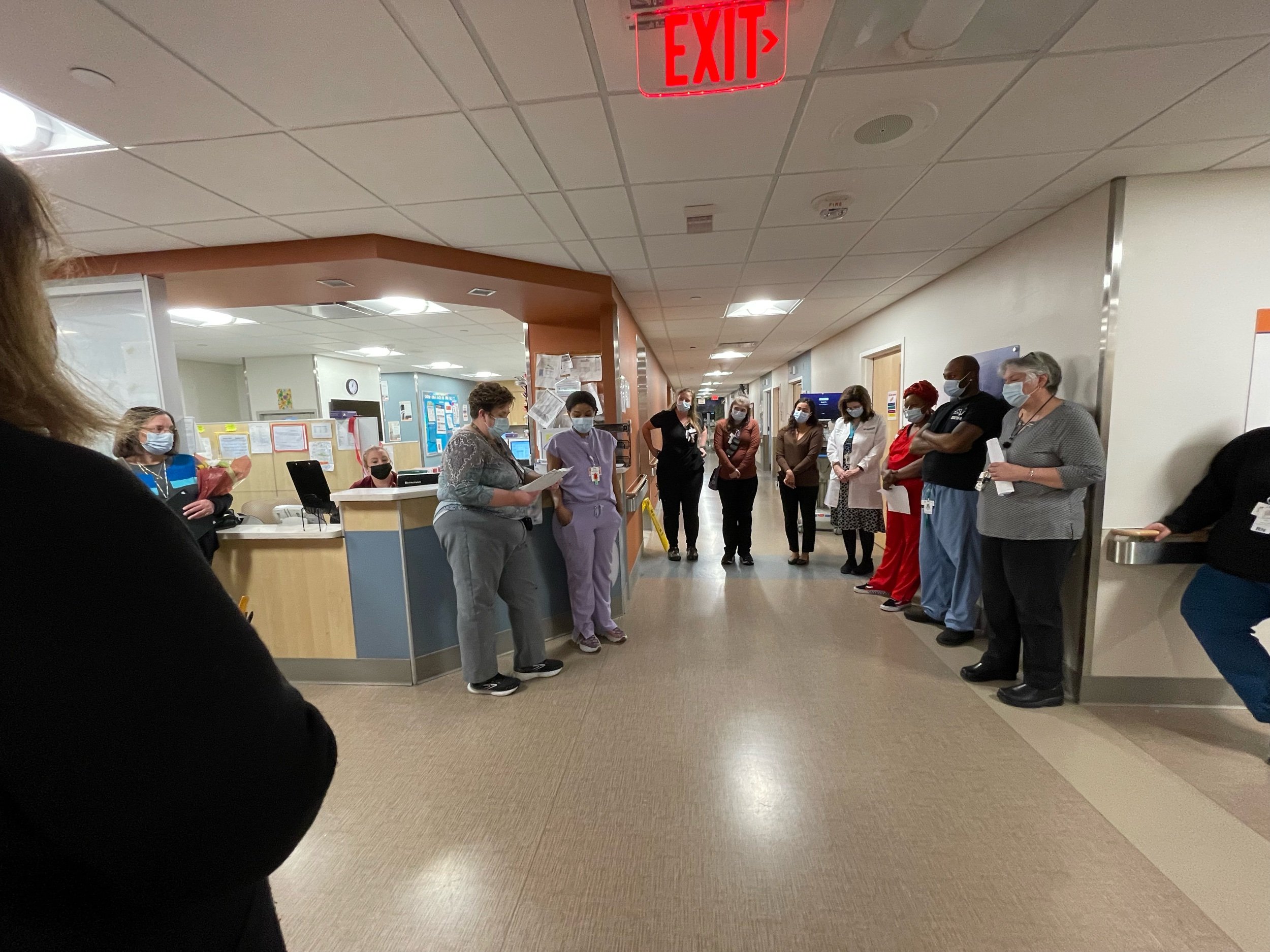
To prioritize the quality of care that we can provide to our patients is one of the central aspects of the fellowship program with SHARE. It was through this fellowship program that I was able to finally leave my own little bubble within the UMass Memorial system and become a part of the entire hospital and network of workers that make up the different departments of our services for patients. I work in an office that is not even on a UMass Memorial hospital campus. This fellowship gave me an opportunity to go into the hospital each week. This was time that I would spend meeting workers from different departments who I had perhaps talked to over the phone or sent an email to already. I got to see so many new faces and build new relationships. Slowly, I even became aware of the problems and challenges that individual employees or entire departments would face. We all face similar problems that take different forms and come at different times. Whether it’s a department that is short staffed, an employee who is working too many hours, or issues with training, these problems are hospital-wide. To see this firsthand, and to see how the employees will try to work with SHARE and management to overcome these issues as they arise, the prioritization of the quality of our care was evident. This fellowship allowed me to become a part of these improvement systems and to learn what it takes to fix a problem from start to end. This fellowship showed me that even in a divided and siloed system, we can work together to help each other. Here at SHARE, we support each other, and we come together to make things better. That’s what a union is supposed to be – it is the meaning of the word itself.
Learning About Negotiation, Every Day
SHARE worked closely with the fellows to provide different exercises to help us better understand and work through various problems at the hospital. We recently finished one of our weekly “Lakeside Learning” sessions where we were given a very in-depth role-playing exercise. We were given information beforehand to help us understand the scenario at hand – interest-based bargaining for a teacher's union. To go through this exercise, some of us were placed on the union side, while others were told to take on the role of management. It was a lot of fun to watch them go back and forth and take on a persona that is so out of their character. By the end of this exercise, we had come to an agreement. After a lot of fighting, after a lot of genuine frustration on both ends, we were able to come to a compromise that emphasized our interests. We came to realize that what both sides wanted so badly was the same thing, and it was all within reach through proper communication and a little bit of patience... I might have jumped the gun a couple of times without having all the information and just automatically, you know, tried to stick up for that a person on my team. We all left the session with many tips and tricks to help us maneuver through these difficult situations while also making sure that everything is talked about that needs to be addressed.
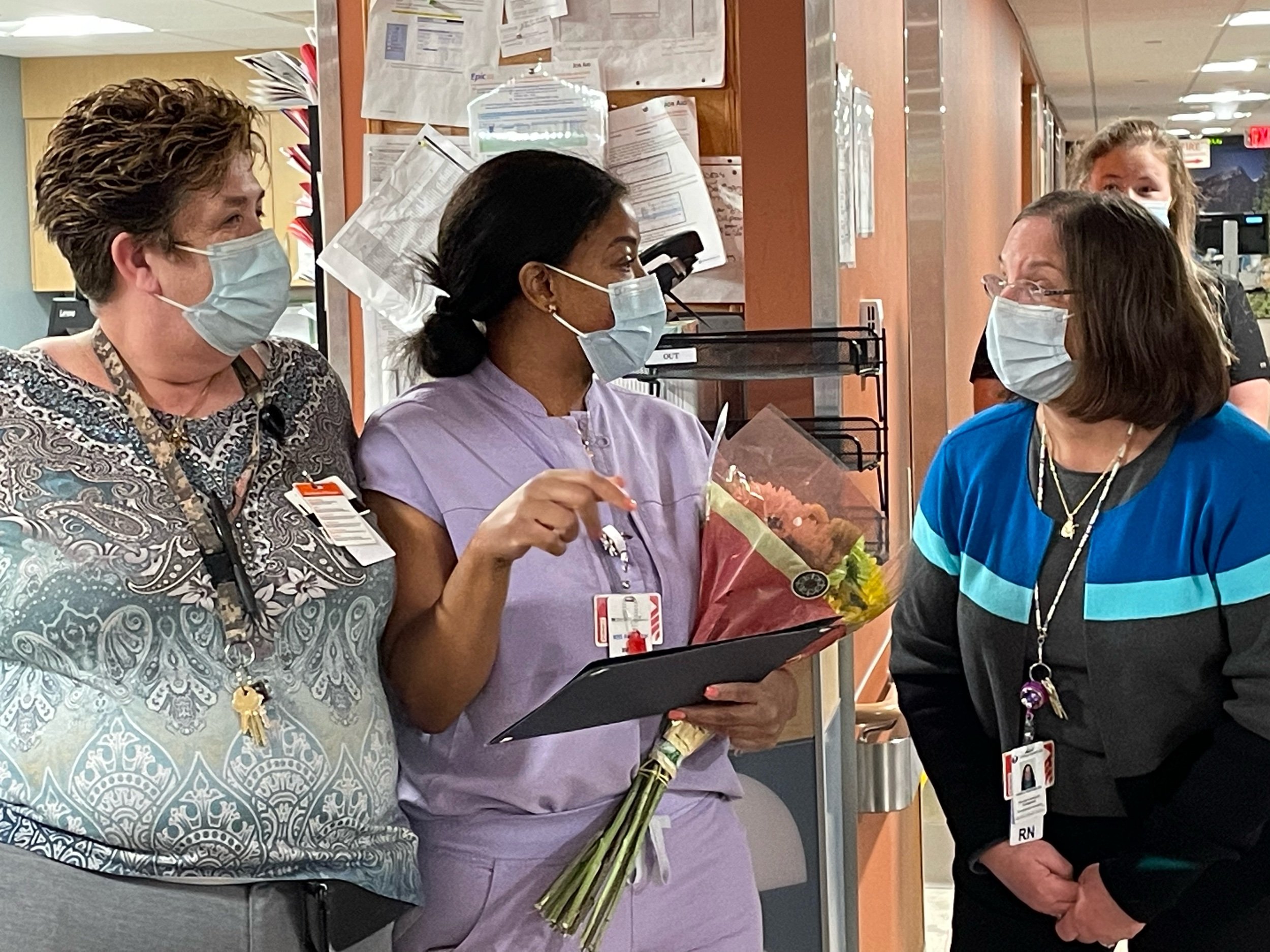
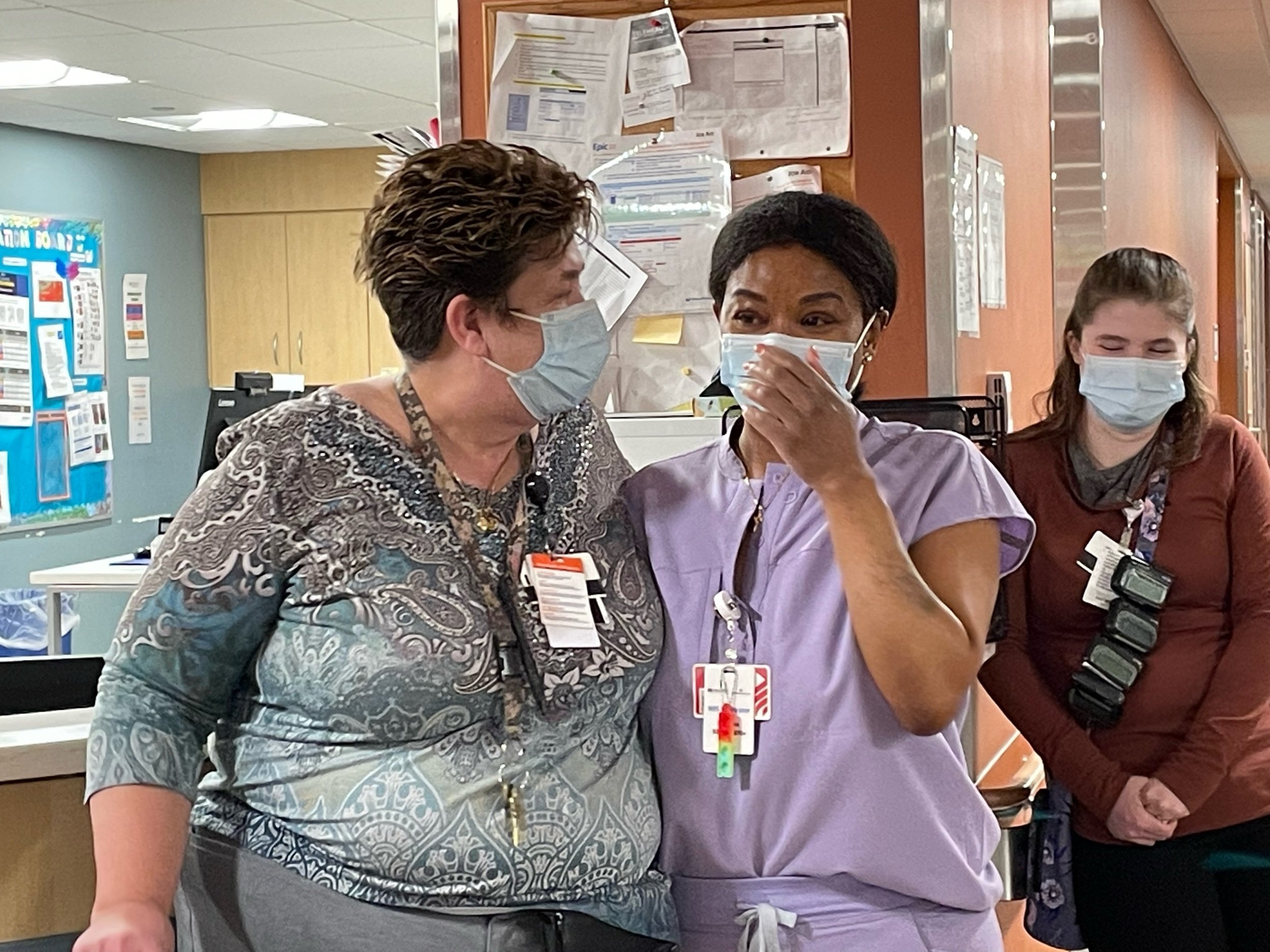
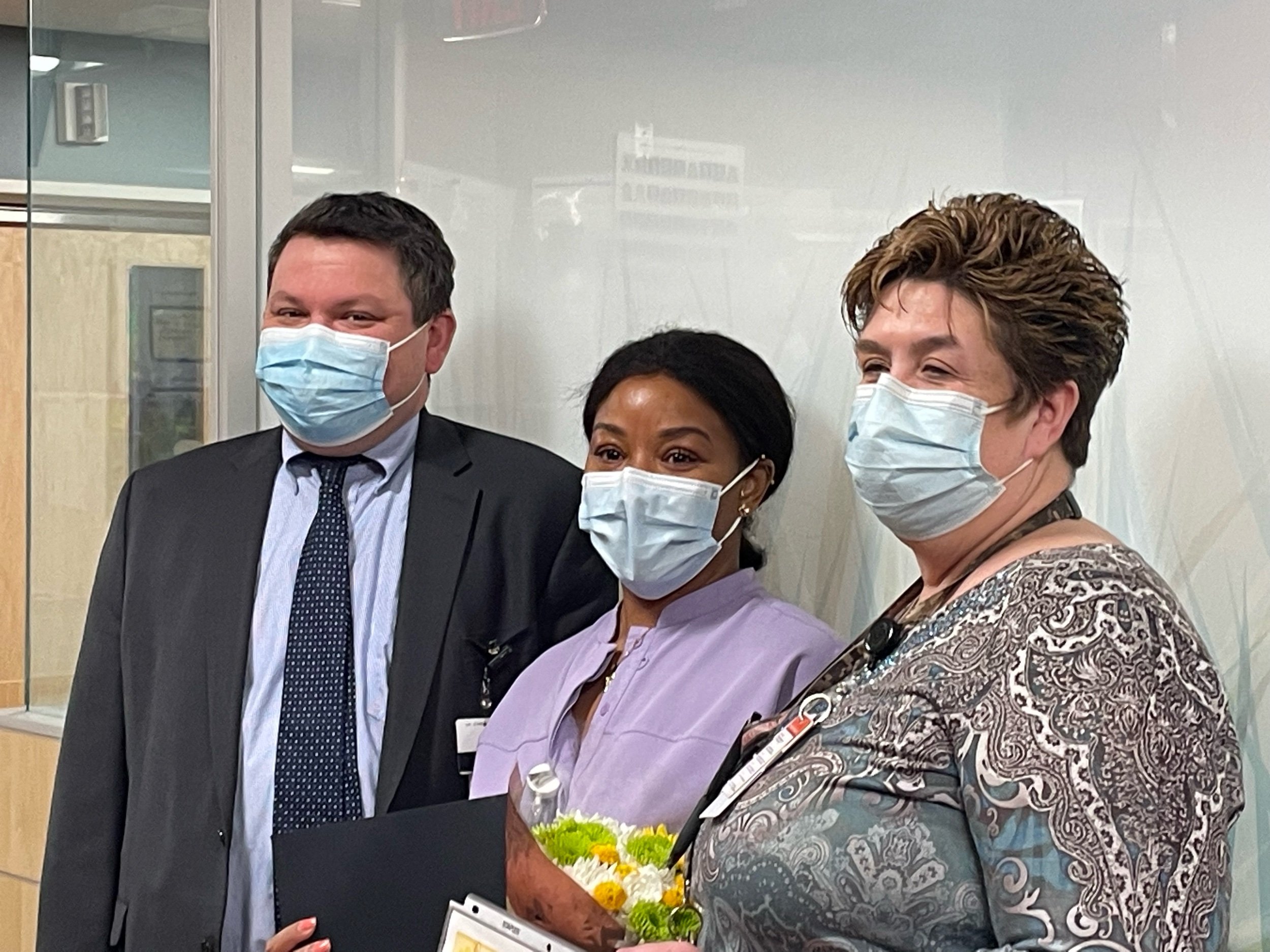
My time with this fellowship is something that I will hold near and dear to my future with Memorial Hospital and SHARE. I was recently nominated to be an E-Board member, so as I take that next step, I have made it very clear to SHARE that they’re not getting rid of me just yet. I have told them that I am going to inject myself into any aspect of helping and organizing that is going on in the hospital. I feel very lucky to have been allowed this opportunity, and that the timing to make such a commitment worked out well. I still remember the day that I became a rep, and how Will Erickson had scouted me out to get involved before I even became a SHARE member. When he first told me of the fellowship program that they were going to launch, I was not yet ready to do it. My department was short-staffed, and I did not want to leave my team with more work. Fortunately, I have a great relationship with my management, and they immediately recognized the value of what this program could offer to workers and their departments. They told me, ‘Tameka, if this is something that you think will help you, and will help you improve our department, then please take the time to do it.’ Eventually, SHARE and my management were able to work closely to figure out a schedule that would not put too much of a strain on our staff. I am excited to fully return to my team, and I’m excited for others to take on this fellowship and learn everything that I did. I will always miss my weekly routine of going into the hospital and seeing who we could help and who we could talk to, but I now know that I can make as much of an impact through my individual role at the hospital.
A Delicate Balance in the nicu
My role in the hospital is to make sure that all the patients that come in through the emergency room are properly insured, and that their insurance information is properly recorded. Currently, I have been assigned to work specifically with mothers with newborns that are kept in the hospital. I make sure that everything is insured so they don't get bills and the hospital gets paid and everybody is happy, and you know everyone gets paid for their good work and patients don't have to worry about missing a bill. When a mother has a newborn child that is sick and in the NICU, the last thing they’re going to be thinking about is whether their insurance coverage has been filled out properly. When I first call these patients, it is important for me to be very sensitive and cautious about how I get all this information from them. I do not want to add any additional stress onto what a situation that is already highly sensitive.
I was originally a CNA before taking on this separate role at the hospital, so I am familiar with patient care. I know how to deal with patients hands on, so that's why it's easy for me to, in the background, be very sensitive to them while also getting the job done. To be mindful of something so simple can relieve a lot of stress for patients down the line. Whenever I get the call that a patient has their baby in the NICU I will typically give the mother a few days to get settled into the challenge that they’re going through. It is sometimes impossible for a mother to understand the questions that I would have to ask them when their child is going through something that they might not understand. It is a very difficult balance to maintain, because at the end of the day, if we do not get the payments through the insurance companies, and the insurance companies do not get their payments, then the whole system would fall apart. I try my best to make the patients feel as if the insurance is not what matters to us, because at the end of the day, it's not. What matters to us at the hospital is to do everything we can to provide the highest quality of care to our patients. I want them to feel that when they get a call from me.
Taking Care of Patients & Taking Care of Ourselves
More than ever before, because of the pandemic, we had to take care of one another this year. We had to make sure that no one was being overworked, underappreciated, or left without any support here at the hospital. By the end of the fellowship, I came to understand that the workers must be taken care of, just as we take care of our patients with such high standards. What it boils down to is that the patients must be taken care of, and the patients cannot be taken care of if the workers are not taken care of too. It's about making sure that our people are cared for because, you know at the end of the day, these people are sent out into the world to care for others in whatever fashion it is. Whether it's health care, whether it's education, or anything else that focuses on providing a selfless service to others, you can't expect them to do their best if they're not taking care of too. They have to be taken care of too.